How diabetes can affect your eyesight
Updated July 2024 | 5 min read
Expert contributors Yu-Yun Wang, managing optometrist at HCF Eyecare; Professor Peter van Wijngaarden, deputy director and head of ophthalmic neuroscience at the Centre for Eye Research Australia
Words by Beth Wallace
For the growing number of Australians diagnosed with diabetes each year, it’s important to understand the risk of eye disease – and how to avoid it.
According to a 2022 report by Diabetes Australia, the number of people with diabetes around the country has surged over the past two decades, from 459,678 in 2000 to more than 1.47 million in 2022 – an increase of about 220%. At this rate, the report predicts, there will be more than 3.1 million Australians living with diabetes by 2050.
While there’s an awareness that diabetes is on the rise, it's less well known that people have a high risk of developing eye complications from diabetes and, if left untreated, can lead to poor vision and blindness.
The good news is that most serious vision loss from diabetes can be prevented, says Professor Peter van Wijngaarden, deputy director and head of ophthalmic neuroscience at the Centre for Eye Research Australia.
“About 90 to 95% of all vision loss and blindness from diabetes is preventable through tight control of blood glucose, blood pressure and blood lipids cholesterol levels, combined with regular screening eye tests,” he says.
Diabetes and eye health
Diabetes occurs when your body loses the ability to produce insulin or stops producing or using it efficiently. This causes blood glucose levels to rise.
Over time, high blood glucose levels damage your blood vessels, which can lead to heart attack, stroke and problems with the kidneys, gums, feet and nerves.
High blood glucose levels can also negatively affect your eyes in several ways. To begin with, they can trigger changes in the shape of the lens, consequently blurring your vision. Persistently high glucose levels increase the risk of developing cataracts, macular oedema, glaucoma and dry eyes.
Diabetes can also damage the small blood vessels, called capillaries, in the retina. If they rupture, small bleeds and swelling occur at the back of the eye. The medical name for this is diabetic retinopathy.
Prof van Wijngaarden explains that diabetic retinopathy is the most common cause of avoidable vision loss and blindness in working-age Australians – and anyone with either type 1 or type 2 diabetes is susceptible. “The risk is related to how long you’ve had the disease – increasing significantly beyond about 10 to 15 years – and how well the diabetes has been managed,” he says.
He points out that women with gestational diabetes are at minimal risk of developing diabetic retinopathy. However, pregnant women with type 1 or type 2 diabetes should have an eye check early in their pregnancy and may need to be monitored closely, because pregnancy can accelerate the progression of diabetic retinopathy.

What are the symptoms to look out for?
There are no specific symptoms for diabetic retinopathy, says Yu-Yun Wang, managing optometrist at HCF Eyecare, which is why it’s so important to book regular diabetic eye checks with your optometrist.
“In the early stages of the condition, you don't notice any changes to your vision,” he says. “It's usually at the middle or the late stage when you'll notice your vision is not great. You may experience blurred or double vision, smudges in your vision, or sensitivity to light. Usually by that point, you'll need surgical intervention.”
Even though you typically won’t experience any symptoms early on, your optometrist will be able to diagnose a range of issues by monitoring changes to your eyes, he adds.
“Given the very fine vascular structure of the back of the eyes and how accessible it is in viewing it, the eyes can give invaluable information on the general status of the patient as well as ensuring there are no damages or changes to the back of the eye, especially the retina.”
Treatments and prevention
The earlier that eye disease can be detected, the easier it is to treat – and the better the outcome, including a reduced risk of vision loss and blindness.
Diabetes Australia recommends having your eyes checked when you’re first diagnosed with diabetes, and then at least every two years after your diagnosis. Diabetes eye tests are bulk billed to Medicare, so there are no out-of-pocket costs.
HCF Eyecare Centres also provide free eye checks for members through the More For Eyes* program. Members on eligible extras cover can claim 100% back on a selected range of prescription glasses or contact lenses, and one free retinal image. To find More for Eyes providers, find a participating provider on our website.
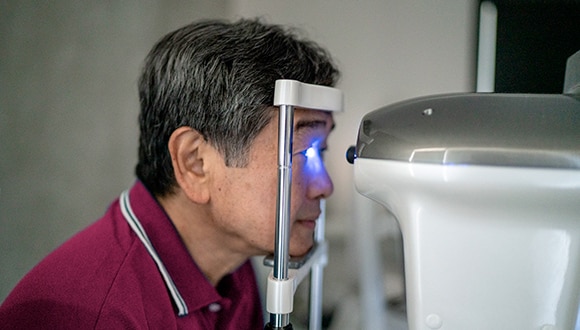
During a diabetes eye check, Yu-Yun says drops are put in the eyes to give a comprehensive assessment of the retina and back of the eye.
“What we’re looking for is any bleeds or changes to the retina,” he explains. “The patient’s vision will be blurry for one to three hours after the eye test, so we advise them in advance, as we don’t recommend driving afterwards.”
If any issues are detected, you may be referred to an ophthalmologist. Also known as an eye surgeon or eye doctor, an ophthalmologist is a medical doctor specialising in the diagnosis and management of eye disorders, such as diabetic retinopathy.
The main treatment for macular oedema, which is a complication of diabetic retinopathy, is intravitreal injection, which involves the injection of a medication into the eye. Prof van Wijngaarden says it’s a highly effective way to improve vision and has “transformed” patient care, but requires a commitment to get monthly injections, sometimes for many months.
Meanwhile, ophthalmologists can perform retinal laser treatment to slow the progression of diabetic retinopathy and limit vision loss. Surgery may be needed if the condition is already advanced by the time of diagnosis.
How to improve eye health
Just as a healthy lifestyle helps control other risk factors associated with diabetes, maintaining a healthy weight, eating a well-balanced diet, exercising regularly and not smoking are essential for preventing, or slowing down the progression of, macular oedema and diabetic retinopathy. Similarly, scheduling regular health checks with your GP and other health practitioners can help identify any issues early on.
“By managing the diabetes, it will reduce the risk of all the problems associated with the disease, including the eyes,” says Yu-Yun.
Registering with the government-funded KeepSight program is a great way to keep on top of your diabetes eye test appointments.
“It’s a free program managed by Diabetes Australia that provides a convenient reminder when your next eye check is due,” says Prof van Wijngaarden. “At the moment, we've got 440,000 people registered, which is about one-third of all Australians with diagnosed diabetes, and we're working towards getting everyone on the registry.”
He explains: “Often diabetic eye changes occur over a longer period but sometimes it can change quite rapidly, so having regular checks and coming back early if you feel there is anything unusual with the eyes is important.”
Coaching support for diabetes
If you have diabetes and need support to improve your health, HCF can help you manage your condition with The COACH Program®. Delivered by qualified health professionals, this telephone support program is provided by health coaches, at no extra cost for eligible members^ with heart conditions or diabetes.
Related Articles
Can you reverse pre-diabetes?
Lifestyle changes can reduce the risk of people with pre-diabetes developing type 2 diabetes. Find out what to do.
Living with a chronic disease
Being diagnosed with a chronic illness can be an emotional and challenging time, but your mindset can have an impact on how you cope.
What is gestational diabetes?
Despite coming with serious risks, you can manage gestational diabetes with the help of your GP and medication if you need to.
Diabetes: Signs and symptoms
Are you thirsty, tired and spending a lot of time in the bathroom? These could be diabetes symptoms – but there are ways to treat and live with the condition.
IMPORTANT INFORMATION
* Waiting periods and annual limits apply. 100% back available on selected covers for prescription glasses and sunglasses, and contacts. Excludes add-ons like high index material, coatings and tinting.
^ Eligibility criteria applies. For more information see hcf.com.au/coach
This communication contains information which is copyright to The Hospitals Contribution Fund of Australia Limited (HCF). It should not be copied, disclosed or distributed without the authority of HCF. Except as required by law, HCF does not represent, warrant and/or guarantee that this communication is free from errors, virus, interception or interference. All reasonable efforts have been taken to ensure the accuracy of material contained on this website. It’s not intended that this website be comprehensive or render advice. HCF members should rely on authoritative advice they seek from qualified practitioners in the health and medical fields as the information provided on this website is general information only and may not be suitable to individual circumstances or health needs. Please check with your health professional before making any dietary, medical or other health decisions as a result of reading this website.